Congenital Differences Learning Center
Often, as children develop in the womb (in utero), they may develop extra fingers, they may not fully separate their fingers, or they may acquire a whole host of either genetically preprogrammed or idiopathic (no known cause) differences. The most common congenital difference in the upper limbs is syndactyly, where the fingers do not separate.
Congenital 101: Basic Embryology
The period between conception and formation of all of the major body parts is known as embryogenesis. In humans, the growing child is called an embryo up to the 8th week, after which time it is called a fetus. There are many embryologic origins for a congenital amputation (transverse deficiency): symbrachydactyly, ulnar deficiency, radial deficiency, hypodactyly, etc.
Pediatric Trigger Finger
While trigger thumbs in children and adults are similar in etiology and treatment, trigger fingers in children are not the same as in adults. Often, there are anatomic variations that contribute to the triggering in a finger and therefore simple A1 pulley release can fail to relieve the triggering in many cases.
camptodactyly
Camptodactyly comes from the Greek words for bent (kamptos) and finger (daktylos), and is the term used to describe a flexion contracture of the proximal interphalangeal joint (PIP joint) of the fingers, most commonly the small finger. There are 3 main types, Congenital, Acquired, and Syndromic. The Congenital type has the best prognosis, and tends to improve, although not necessarily completely resolve with stretching and splinting. The Acquired type presents in early to late adolescence and is progressive. Splinting and stretching may help to slow or halt progression of the contracture, but correction of the deformity is rate without surgery. Even surgery has a limited success rate. Although there are many surgical options and algorithms that have been described, we prefer a simple 2 flap Z-plasty and FDS tenotomy. Another option which is very powerful but requires patient buy-in is the digit widget. All surgical options suffer from a high recurrence rate. Syndromic camptodactyly can be associated with a wide variety of disorders, including Arthrogryposis.
rotational osteotomy for Forearm synostosis
Congenital synostosis of the forearm is generally well tolerated, as most children are born with their forearms stuck in a neutral position. For children with a moderate to severe forearm pronation or supination contracture, a rotational osteotomy can set forearm rotation to a more useful position. We recommend somewhere between 15 and 30 degrees of pronation. Compartment syndrome is a risk, particularly with correction of more severe deformities. We therefore recommend a slight shortening of the forearm to relieve some of the tension that arises from rotating the forearm, analogous to wringing a towel.
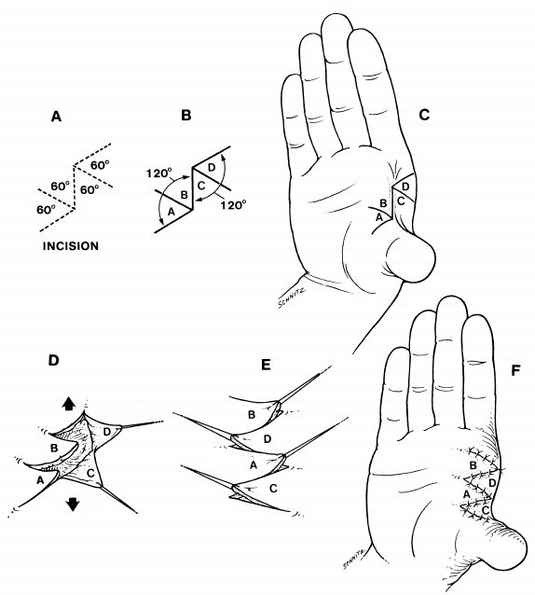
4-Flap Z-plasty
A tight first web space (between the thumb and index finger) is common to many congenital conditions. Having the thumb and index finger too close together can make it hard to pinch, shake hands, and grab larger objects like bottles. Early treatment includes splinting and stretching exercises. If non-surgical methods have not worked, there are a multitude of surgical options to improve width of the first web space. The most common option is the four flap Z-plasty, which is sometimes combined with a tendon transfer and ligament reconstruction, but in some cases may be sufficient by itself.
Thumb hypoplasia
Radial longitudinal deficiency (see section below) affects the growth and formation of all radial-sided structures, and can result in a small or absent radius as well as a small or absent thumb. The medical workup for radial deficiency is covered in the section on radial longitudinal deficiency. Management of thumb hypoplasia depends on how hypoplastic the thumb is. The Bauth classification helps to determine the severity of thumb hypoplasia, and guides treatment.
Type I Thumb Hypoplasia: The thumb is fully functional, but is slightly shorter compared to the other side.
Type II Thumb Hypoplasia: The thumb is small, but is also missing intrinsic muscles (thenars, adductor, flexor pollicis brevis). There may also be a pollex abductus, an aberrant connection between the flexor pollicis longus (FPL) and extensor pollicis longus (EPL) that limits flexion/extension motion at the thumb metacarpophalangeal (MP) joint and also abducts the joint. The first web space is tight, and the ulnar collateral ligament (UCL) of the MP joint is incompetent. Occasionally, the radial collateral ligament may also be compromised. Babies and toddlers will usually incorporate a type II thumb into hand function for both pinch and grasp. Treatment is with oppositionplasty and UCL reconstruction to replace the function of the thenar muscles and to stabilize the MP joint.
Type III Thumb Hypoplasia: The thumb is small, and is missing both intrinsic and extrinsic muscles (FPL, EPL). The MP joint is grossly unstable. If the thumb carpometacarpal (CMC) joint is intact, the thumb is considered a Type IIIA. If the thumb CMC joint is unstable or absent, that is a Type IIIB thumb. Type IIIA thumbs can be functional and incorporated into grasp, but rarely used for pinch. Type IIIB thumbs are typically ignored by the child and not used for pinch or grasp. Type IIIA thumbs can be reconstructed with oppositionplasty and MP fusion, as well as other tendon transfers as needed. Type IIIB thumbs can either be replaced or reconstructed by transferring a second toe from the foot, or replaced with an index finger pollicization. While a pollicization provides better function than a toe to thumb transfer, it does leave the child with 4 digits instead of 5, which may not be acceptable in certain cultures or to some parents.
Type IV Thumb Hypoplasia: This is known as a Pouce Flottant, a “floating thumb.” In place of a thumb, the child has a skin tag connected to the radial side of the hand only by a skin bridge conveying an artery, veins, and a nerve. The child will completely functionally ignore the thumb.Type IV thumbs can either be replaced or reconstructed by transferring a second toe from the foot, or replaced with an index finger pollicization. Function is markedly better with a pollicization.
Type V Thumb Hypoplasia: Complete absence of the thumb. Type V thumbs can either be replaced by transferring a second toe from the foot, or by an index finger pollicization. Function is markedly better with a pollicization.
Pollicization and thumb ablation with vascularized fat transfer
For children born with an absent or deficient thumb, index finger pollicization (making into a thumb) restores much of the function and appearance of a thumb.(1,2) The decision to ablate an existing but deficient thumb is never easy for parents. However, if the child bypasses the thumb and uses the index finger for pinch and grasp, they are telling us that their brain does not perceive the thumb as a functional thumb, instead having shifted the "thumb" part of the brain to the index finger. The technique is complex (3) and should only be attempted by surgeons with specific expertise in politicization. Typically, children remain in a cast for 4 weeks after surgery, after which 2 months of therapy and splinting are required.
Radial longitudinal deficiency (radial club hand)
Children born with an absent or shortened radial forearm bone are considered to have a radial longitudinal deficiency. If the wrist is radially deviated, this position is called a radial club hand. Radial deficiencies can be either idiopathic (no known cause), inheritable (passed on from parent to child), or due to teratogens (toxins that affect fetal development). Inheritable causes include Fanconi Anemia, Holt-Oram Syndrome (aka Heart-Hand Syndrome), Thrombocytopenia Absent Radius (TAR), and Diamond-Blackfan Syndrome. Radial deficiencies usually affect other organ systems that form embryologically at the same time, as can be seen with VACTERL Association.
All children with radial deficiencies should have:
1) Radiographs of the spine to rule out congenital spine deformities
2) A renal ultrasound to rule out kidney disorders
3) An echocardiogram to rule out heart disorders
4) Blood taken for a CBC to look for anemias
5) Genetic testing to rule out inheritable causes as listed above including a Chromosome Fragility Test
Once all of the potential comorbidities are identified and stabilized, the radial deficiency itself can be managed. There are as many opinions about how to best help children with radial deficiencies as there are surgeons who treat it. For the radial club hand, there are 6 basic treatment options:
1) Stretching only. Children with radial deficiencies will have a high level of function, and unless they have both sides involved and both sides are too short to reach their mouths or to allow wiping after the bathroom, they will be independent in life. No surgery has yet demonstrated an improvement in function after surgery, and no surgery has been reliably able to restore the appearance of the hand back to “normal.” A diligent stretching program with committed parents and a knowledgeable therapist can produce results equivalent to surgical release.
2) The bilobed flap. The bilobed flap procedure can make the wrist a little less tight and easier to stretch. This is a skin rearrangement and tendon releasing operation that can be done as an outpatient and has minimal risk.
3) Centralization. This is the classic and oldest technique for placing the hand in line with the forearm. The middle finger is placed on top of the ulna and soft-tissue structures are released on the radial side of the arm. Modifications of this technique include using an external fixator to stretch the soft tissues before transposing the hand on the ulna, allowing the wrist to sit on the end of the ulna without having to remove a part of (notch) the central bones of the wrist. Notching has been shown to decrease recurrence of the deformity, but also to decrease joint motion at the wrist.
4) Radialization. In an effort to minimize recurrence, the Centralization technique was modified to place the index finger in line with the ulna and to transfer all radial sided tendons to the ulnar side of the wrist.
5) Ulnarization. To further limit recurrence of the radial club hand deformity, ulnarization places the hand all the way over on the opposite side of the ulna. The ulna can often become prominent, leading to a visible bony bulge in the place where the thumb would be. The results of this technique have been mixed, with some excellent and some poor results.
6) Free tissue transfer. Developed by Simo Vilkki in Finland, the vascularized free toe joint transfer known as the Vilkki Procedure has shown some great results. However, the procedure requires sacrificing a toe joint and spending a few days in the hospital.
Syndactyly
Syndactyly, fingers joined together at birth, is the most common congenital difference. The developing embryo first grows a hand paddle, with all of the fingers attached (Figure 1). By the 8th week of development, the fingers separate and clefts are created between the fingers. In some children, those cleft either do not form or do not complete the separation, resulting in fingers that are either completely or incompletely stuck together. In fingers that are together but are of different lengths, such as the small and ring fingers, the smaller finger tethers the longer finger and limits it from growing (Figure 2). The fingers may twist around each other as well. Small-ring finger and index finger-thumb syndactyly needs to be released at a young age (as young as 6 months) to minimize the risk of permanent deformity of the fingers and thumb. The most common syndactyly, however, occurs at the long-ring finger web space (Figure 3). Syndactyly can occur as a sporadic, isolated finding or as part of a syndrome or condition (Figure 4). Amnionic bands can bind the fingers, amputating parts and also joining them together (Figure 5).
Polydactyly
Polydactyly means “many fingers,” and is a term used to describe the condition where a child is born with more than 5 digits on each hand or foot. Postaxial polydactyly Type B is the most common, particularly in children of Sub-Saharan African ancestry, where it is passed on as an autosomal dominant trait. That means that if a parent has it, each of their children has a 50% chance of having it. Postaxial polydactyly type B can occur in both hands or only in one. These ‘nubbins” are often tied off in the nursery, which we do not recommend as about a quarter of these can have complications. It is also difficulty for the family to watch the nubbin swell and turn purple, eventually turning black and falling off. Our technique of removal in the office is virtually painless (only the injection of local anesthetic) and we have not had any complications from it so far (see video). Not all postaxial polydactyly type B fingers can be safely removed in the office. If the base of the digit, the stalk that connects the nubbin to the rest of the hand, is more than 1/8th of an inch wide, we recommend removal in the operating room to get a better result.
Postaxial polydactyly type A is a nearly or fully formed extra digit, most commonly associated with genetic disorders such as Ellis-van Creveld Syndrome. These larger extra fingers need to be removed in the operating room under general anesthesia.
Ulnar deficiency
Far less common than radial deficiency, hypoplasia or aplasia of the ulnar side of the arm can vary greatly in presentation. Phocomelia (flipper-like arm), that resulted from thalidomide use in the 1950’s and 60’s in Europe, is now believed to have been a severe form of ulnar deficiency. Unlike radial deficiencies, there is no known associated internal organ system involvement. Other associated musculoskeletal issues include scoliosis, proximal femoral focal deficiency (PFFD), and fibular hemimelia. The cause of ulnar deficiency is thought to be a sporadic loss or weakening of the zone of polarizing activity in the developing limb (see CONGENITAL 101). Most of the time it involves only one side and is not thought to have a genetic cause. However, when the chest is also affected, the child may have Ulnar-Mammary or Schinzel Syndrome. Schinzel Syndrome is due to one of two known genetic mutations, and is therefore inheritable.
Cleft hand (Ectrodactyly)
Children with cleft hands are born with a gap in the middle of the hand. Most commonly, only the middle finger is absent and the thumb/index web space is tight. Other children may have only one or two fingers, or no fingers at all. The small finger (pinky) is the last to be lost.
Madelung Deformity
Named after Otto Madelung but originally described by Malgaigne in 1855, the Madelung deformity results from restriction of growth of the volar-ulnar corner of the distal radius. “True” Madelungs disease is caused by a Vicker’s ligament tethering the volar-ulnar distal radius growth plate. The Vicker’s ligament is an aberrant short radiolunate ligament that originates from the metaphysis rather than the epiphysis. Similar aberrant ligaments occur elsewhere in the body, including the distal ulna. In the distal ulna, the deformity has been called Focal Fibrocartilaginous Dysplasia (FFD), although some believe that FFD is a unique dysplasia unrelated to Madelung deformity. Other cases of growth arrest at the volar-ulnar corner of the distal radius that can mimic Madelung disease include Multiple Hereditary Exostoses (MHE), Gymnast Wrist, and distal radius physeal fractures. Only Madelung Disease has a Vicker’s ligament. Leri-Weil Dyschondrosteosis is an autosomal dominant condition due to a mutation in the SHOX gene that manifests with bilateral Madelung deformity, mesomelic short stature, scoliosis, tibial bowing, a high arched palate, and increased muscle mass. Children with Leri-Weil typically have a Vicker’s ligament and are the archetype for the disease.
Patients typically present in adolescence with a short forearm, prominence of the distal ulna, and a dorsal hump at the wrist. Severe deformities can appear to have the hand attached to the side of the forearm. Pain is common, particularly with repetitive activities. Some patients are unable to participate in sports that require weight bearing of the upper limb. A history of gymnastics should raise suspicion for a Gymnast Wrist and history of a wrist fracture can precede a growth arrest.
Bilateral X-rays of the wrist and forearm are required to assess for distal radial deformity and the so-called “entire radius” variant. Minor deformities with good coverage of the lunate and good motion of the forearm and wrist typically can be managed with serial radiographs every 6-12 months, depending on age. Siblings of children with Madelung Deformity due to tumor or a Vicker’s ligament should be screened for deformity with X-rays every 6-12 months as well. Any patient 10 years old and younger with minor changes in the distal radial physis on X-ray should undergo an MRI to assess for the cause of the changes. Children with Leri-Weil do not require an MRI, as they can be assumed to have a Vicker’s ligament. An MRI may be useful to determine the cause of the deformity, which is fairly reliable in showing not only the Vicker’s ligament, but also tumors and physeal bars.
Treatment can range from observation to complex multiple osteotomies. The goals of treatment are to 1) restore coverage and alignment of the lunate in the radicarpal joint, 2) restore axial alignment of the hand and wrist on the forearm, 3) correct gross deformity of the wrist, and if possible 4) restore DRUJ stability. Achieving these 4 goals typically resolves the child’s pain. Once changes in the distal radius are visible on X-ray, there is some urgency to remove the cause and restore unimpeded growth as soon as possible. That may require removal of the tumor, physeal bar, or Vicker’s ligament, depending on MRI findings. Vicker’s ligament release and radial physiolysis(1,2,3) has shown potential to improve mild deformities when performed in children with at least 4 years of growth remaining.
For children with moderate deformities or older children, a dome osteotomy with or without ulnar shortening may be needed to achieve the treatment goals. Epiphysiodesis of the distal radius and/or ulna may also be required to prevent worsening of the deformity. More severe deformities, particularly if the entire radius is affected, are best managed with multiple osteotomies. The planning of multiple osteotomies is extremely difficult to do freehand, and is better managed using 3-D CT scans and computer modeling.
Long-term outcomes of Madelung deformity are unknown, although arthritic changes may be more common than has been reported, particularly in patients with poor lunate coverage and high radial inclination angles.
Macrodactyly of the thumb and index finger.
Hemihypertrophy
macrodactyly and hemihypertrophy
Some children are born with an overgrowth of the hand (macrodactyly) or even the entire arm (hemihypertrophy). While the causes of macrodactyly and hemihypertrophy are not well understood, we do know that there is an association with nerve tumors called lipofibromatous hamartomas. There is also an association with Wilm’s tumors, particularly in hemihypertrophy. Wilm’s tumors are tumors of the kidney also called nephroblastomas, and are the most common kidney tumors in children. Children with hemihypertrophy should be screened with an abdominal ultrasound every 3 months until the age of 8, and with bloodwork to assess alfa fetal protein (AFP) levels every 6 weeks until 4 years of age.
We do not recommend treatment at a young age for mild macrodactyly or hemihypertrophy that does not cause pain or dysfunction. In certain instances, where the overgrowth is limited and mild enough to allow us to recreate the typical appearance of the arm and hand, we do recommend surgery to correct any bony or soft tissue deformities. For children with more severe involvement, treatment can range from debulking, to stopping the growth of the bones (epiphyseodesis), to amputation.
Congenital Coronoid Insufficiency
The elbow is not a simple hinge joint. There are actually 3 joints that make up what we think of as the “elbow joint.” The most conforming and therefore most restrictive joint is the ulno-humeral joint. The joint at the distal humerus is shaped like a spool (Figure 1), with a tightly conforming counter-shape on the proximal ulna (Figure 2). The radiocapitellar joint is shaped to allow rotation about the axis of the center of the radial head and to allow gliding rotation centered on the center of the capitellum. The capitellum is convex, and the radial head is concave, conferring some stability to the joint (Figure 3). The third joint is the proximal forearm joint formed between the radial head and the proximal ulna (Figure 4).
The primary bony stabilizers of the elbow are the coronoid and the radial head, as well as their counterparts at the distal humerus. Some children are born without a coronoid (Figure 5) and may have a deficient radicapitellar joint as well. Without the primary bony stabilizers, the elbow often dislocates when it goes into extension beyond 60-45 degrees. Long-term consequences of daily and sometimes minute-by-minute dislocations can be arthritis and deformity. There has historically been no reliable way of restoring stability to these elbows. However, recent advances in computer technology may offer a possible solution. With the aid of 3-D computer simulation software (Figure 6), it is now technically possible to replace the coronoid with the patients own bone from another part of the elbow (1,2).